Ribbon partners with a leading health plan subsidiary to significantly improve provider data accuracy and member experiences
For health plans laser-focused on improving member experiences and health outcomes, inaccurate provider data can be a major roadblock to success. Plans wrestle with legacy systems, noisy and outdated data, and manual processes that lead members to struggle with finding an in-network provider and understanding costs ahead of time.
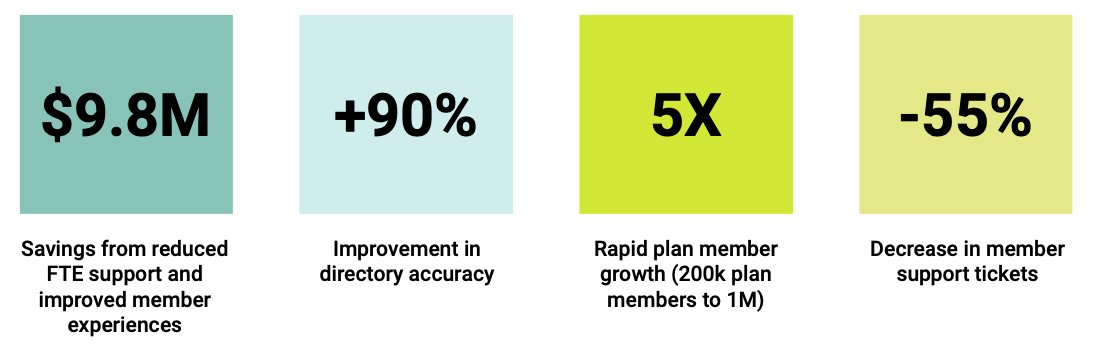
Download the case study to learn why one leading health plan brought Ribbon Provider Data Platform on board, how Ribbon integrated into their systems, and how they were able to improve their provider directory accuracy by 90%.